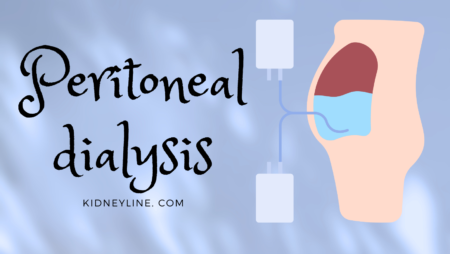
Peritoneal dialysis is a treatment option for individuals with kidney failure. It is a way to help the body get rid of harmful toxins when the kidneys can no longer perform that function.
Patients can perform this procedure themselves or with the help of a caregiver or healthcare professional. However, it is important to note that peritoneal dialysis requires a strict schedule and adherence to hygiene practices to prevent infection.
What is Peritoneal Dialysis
Peritoneal dialysis (PD) is a type of dialysis that uses the peritoneum, a membrane lining the abdominal cavity, to filter waste and excess fluid from the blood. Unlike hemodialysis, which requires a machine to filter the blood outside of the body, peritoneal dialysis uses the body’s own natural filtering mechanism.
During peritoneal dialysis, a sterile solution called dialysate is infused into the peritoneal cavity through a catheter. The dialysate then sits in the cavity for a set amount of time, allowing waste and excess fluid to pass through the peritoneum and into the solution. After the prescribed time, the dialysate is drained out of the body through the catheter and discarded.
Peritoneal dialysis is often used as a treatment for kidney failure when a patient’s kidneys are no longer able to function properly. It can be performed at home, allowing for greater flexibility and independence for the patient. However, it requires a significant amount of patient education and training to ensure proper technique and infection control.
Types of Peritoneal Dialysis
Continuous Ambulatory Peritoneal Dialysis
Continuous Ambulatory Peritoneal Dialysis (CAPD) is a type of peritoneal dialysis that can be done at home. It involves manually exchanging bags of dialysate fluid several times a day. The patient fills their peritoneal cavity with the dialysate fluid, which then sits for a few hours, allowing waste products to diffuse into the solution. The patient then drains the fluid out and replaces it with a fresh bag of dialysate. CAPD is typically done four to five times a day, with each exchange taking about 30 minutes.
CAPD is a good option for patients who want to maintain their independence and flexibility. Since it can be done at home, patients can continue with their daily activities while receiving treatment. However, it requires a high level of patient compliance and may not be suitable for patients with mobility or dexterity issues.
Automated Peritoneal Dialysis
Automated Peritoneal Dialysis (APD) is a type of peritoneal dialysis that uses a machine to perform the exchanges. The machine, called a cycler, is programmed to perform several exchanges throughout the night while the patient sleeps. The cycler drains the used dialysate from the peritoneal cavity and replaces it with fresh fluid. In the morning, the patient disconnects from the machine and goes about their day.
APD is a good option for patients who want a more convenient and automated option. It requires less manual labor than CAPD and can be done while the patient sleeps. However, it may not be suitable for patients who are sensitive to fluid shifts or have sleep disorders.
Both CAPD and APD are effective types of peritoneal dialysis. The choice between the two depends on the patient’s lifestyle, preferences, and medical needs. Patients should discuss their options with their healthcare provider to determine the best treatment plan for their individual situation.

Benefits of Peritoneal Dialysis
Here are some benefits of Peritoneal Dialysis:
- Convenience: PD can be done at home, allowing patients to have more control over their treatment schedule and avoid the need for frequent visits to a dialysis center. This can be especially beneficial for patients who live in rural areas or have mobility issues.
- Flexibility: PD can be done during the day or at night, depending on the patient’s preference and lifestyle. This can allow patients to continue working, traveling, or pursuing other activities while receiving treatment.
- Better Quality of Life: PD has been shown to improve patient’s quality of life compared to hemodialysis, another type of dialysis. PD is associated with less fatigue, better appetite, and fewer restrictions on diet and fluid intake.
- Lower Risk of Infection: PD carries a lower risk of infection compared to hemodialysis, which requires access to the bloodstream through a catheter or fistula. PD uses a sterile solution that is infused into the peritoneum, reducing the risk of bloodstream infections.
- Cost-effective: PD is generally less expensive than hemodialysis, as it does not require expensive equipment or frequent visits to a dialysis center. This can be especially beneficial for patients who do not have insurance or have limited financial resources.
Overall, Peritoneal Dialysis can be a viable option for patients with end-stage renal disease who are looking for a convenient, flexible, and cost-effective way to manage their condition.
Risks and Complications of Peritoneal Dialysis
Infection
One of the most common risks of peritoneal dialysis is infection. This is because the peritoneal membrane can become infected when the catheter is inserted into the abdomen. Symptoms of infection include fever, chills, nausea, vomiting, and abdominal pain. In severe cases, the infection can spread to other parts of the body, such as the bloodstream, which can be life-threatening.
To prevent infection, patients undergoing peritoneal dialysis should follow strict hygiene practices, such as washing their hands before and after handling the catheter and keeping the catheter site clean and dry. They should also avoid swimming or bathing in unclean water and avoid contact with people who are sick.
Hernia
Another risk of peritoneal dialysis is the development of a hernia. This occurs when a portion of the intestine protrudes through a weakened area of the abdominal wall. Symptoms of a hernia include pain, swelling, and a bulge in the abdomen.
To prevent the development of a hernia, patients should avoid lifting heavy objects and engaging in strenuous physical activity. If a hernia does occur, surgery may be necessary to repair the weakened area of the abdominal wall.
Weight Gain
Peritoneal dialysis can also lead to weight gain, which can be a concern for some patients. This is because the dialysis solution used during peritoneal dialysis contains sugar, which can cause fluid to accumulate in the body. This can lead to swelling, shortness of breath, and high blood pressure.
To manage weight gain, patients should follow a healthy diet and exercise regularly. They should also monitor their fluid intake and follow their healthcare provider’s recommendations regarding the amount of dialysis solution to use.
Overall, while peritoneal dialysis can be an effective treatment for kidney failure, it does carry some risks and complications. Patients should be aware of these risks and take steps to prevent them.
Comparison with Hemodialysis
Peritoneal dialysis and hemodialysis are two of the most commonly used treatments for end-stage renal disease. While both treatments aim to remove waste and excess fluids from the body, there are some differences between the two methods.
Hemodialysis typically requires three sessions per week, each lasting three to four hours. Peritoneal dialysis, on the other hand, is usually performed every day, and each session lasts for several hours. This means that peritoneal dialysis may require more time commitment from the patient, but it can also lead to a more consistent removal of waste and excess fluids.
There are also some differences in the potential side effects and complications associated with each method. Hemodialysis may lead to low blood pressure, muscle cramps, and infections at the site of the access point. Peritoneal dialysis may cause infection of the peritoneal membrane, hernias, or other complications related to the catheter.
Overall, the choice between peritoneal dialysis and hemodialysis will depend on various factors, including the patient’s lifestyle, medical history, and personal preferences. It is essential to discuss the pros and cons of each method with a healthcare professional to make an informed decision.

Patient Eligibility for Peritoneal Dialysis
Not all patients with end-stage renal disease (ESRD) are eligible for peritoneal dialysis.
To be eligible for peritoneal dialysis, patients must meet certain criteria. They must have adequate manual dexterity and cognitive function to perform the dialysis procedure themselves or with the help of a caregiver. Patients with severe cognitive impairment or physical disabilities may not be able to perform the procedure and may not be eligible for peritoneal dialysis.
Patients must also have a suitable peritoneal membrane. The peritoneal membrane must be able to effectively filter waste and excess fluid from the blood. Patients with severe scarring or damage to the peritoneal membrane may not be able to undergo peritoneal dialysis.
In addition, patients must have a suitable living environment. Peritoneal dialysis requires a clean and sanitary environment to prevent infection. Patients who live in unsanitary conditions or who are unable to maintain a clean environment may not be eligible for peritoneal dialysis.
Living with Peritoneal Dialysis
Living with peritoneal dialysis requires a significant adjustment to daily life. Patients must adhere to a strict schedule and maintain a clean environment to prevent infection. However, with proper care and attention, peritoneal dialysis can be a safe and effective treatment option for those with kidney failure.
One of the most significant changes for patients on peritoneal dialysis is the need for daily exchanges. Patients typically perform four to five exchanges per day, each taking about 30 minutes to complete. This requires a dedicated space in the home for performing exchanges, as well as a reliable source of clean water and electricity.
In addition to the physical demands of peritoneal dialysis, patients must also be vigilant about infection control. This includes washing hands before and after exchanges, using sterile technique during exchanges, and monitoring for signs of infection such as fever or redness around the catheter site.
Despite the challenges, many patients find peritoneal dialysis to be a more flexible and convenient option than traditional hemodialysis. Patients have more control over their treatment schedule and can perform exchanges at home or while traveling. Additionally, peritoneal dialysis does not require the use of needles, which can be a significant source of anxiety for some patients.
Overall, living with peritoneal dialysis requires a significant commitment to self-care and attention to detail. However, with proper training and support, patients can successfully manage their treatment and maintain a good quality of life.
Conclusion
Peritoneal dialysis is a viable treatment option for patients with end-stage renal disease who are seeking an alternative to hemodialysis. It offers several advantages over traditional hemodialysis, including increased flexibility, more independence, and fewer dietary restrictions.
While peritoneal dialysis is not suitable for everyone, it is important for patients to discuss their options with their healthcare provider to determine if it is the right treatment choice for them.
Patients should be aware of the potential risks and benefits of peritoneal dialysis and should work closely with their healthcare team to ensure that they are receiving the best possible care.
Overall, peritoneal dialysis offers a promising alternative to hemodialysis for patients with end-stage renal disease. With the right support and guidance, patients can successfully manage their condition and improve their quality of life with peritoneal dialysis.